The Fork Before the Fix
Food sets the physiological baseline that makes therapy and mindset work.
Stress isn’t just in your head.
It’s in your blood.
That’s why you can meditate until your legs go numb, journal until your hand cramps, breathe like a yogi…
and still find yourself in the pantry at night, or losing your temper in traffic.
It’s not a lack of grit. It’s physiology.
Because when your body gets pulled into survival mode, your brain never even gets a chance.
The Lie We’ve Been Sold
We’ve been told stress is a mindset problem.
Calm your thoughts. Fix your perspective. Just breathe.
But the truth is this: the mind follows the body.
If your body is under-fueled, blood sugar unstable, or cortisol surging, your nervous system flips into fight-or-flight. And once that happens, patience, discipline, and clarity go offline.
What feels like failure is just your biology overriding your plans.
Sarah’s Breaking Point
Sarah was a high-performer. She meditated, journaled, even tried breathwork between meetings. On paper, she was “doing the work.”
But most afternoons told a different story:
2:07 p.m. — Her hands trembled over the keyboard. Stomach hollow, heart racing from her third coffee.
2:15 — She told herself she’d “push through.”
2:32 — She was in the office kitchen, tearing open a cookie wrapper, convincing herself it was “just a little sugar.”
7:45 — She was slumped on the couch, scrolling DoorDash, furious with herself for another night of takeout.
Sarah thought it was a discipline problem.
It wasn’t.
Once she rebuilt her meals (lean protein in the morning, slow carbs at lunch, balanced snacks in between) the difference was night and day.
Same woman. Same job. Same stressors.
But no spiral.
Her nervous system had fuel to stabilize, and her brain finally had room to work.
Stress Starts in the Body
Stress feels like worry.
But worry is just the echo.
The origin is biological:
Cortisol and adrenaline flood your bloodstream, sharpening reflexes but leaving you “wired and tired.”
Blood sugar spikes and crashes cut power to your brain’s “traffic lights,” fueling cravings, irritability, and poor decisions.
Chronic stress rewires your hardware (the HPA axis and vagus nerve) so you panic faster and recover slower.
Mindset tools can help.
But if the foundation is cracked, nothing holds.
Nutrition is what regulates the baseline.
The Double Cost of Eating Poorly
Here’s the trap: when you’re stressed, food is often the first place you turn. And it works — but only for a moment.
That pastry or soda feels calming because blood sugar spikes and dopamine fires. For a brief window, the alarm quiets.
Then the crash comes. Blood sugar plummets, cortisol rebounds, and the nervous system feels even shakier. The alarm didn’t go away — it just hit snooze and then came back louder.
That’s the double cost of eating poorly under stress: temporary relief now, heavier backlash later.
On the flip side, steady fuel (protein, slow carbs, nutrient-dense foods) doesn’t give the same instant “ahhh” hit. But it prevents the crash. Your system slowly learns how to settle instead of being whipped around.
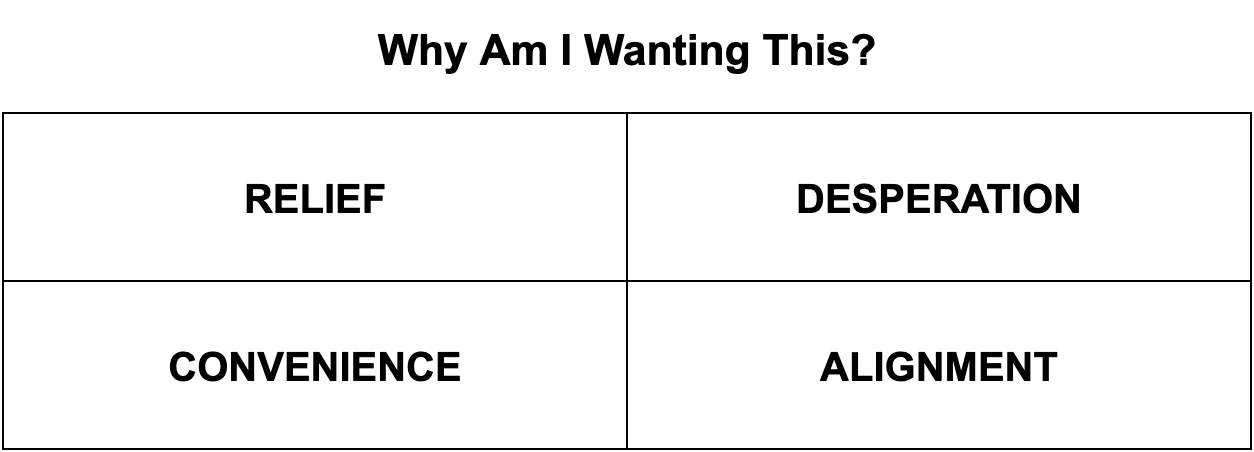
A Better Question: Why Am I Wanting This?
Not all wants are the same. Some are survival signals—the body yelling for quick relief. Others are strategy wants—the mind reaching for what’s fast or familiar. Then there are deeper wants—the ones aligned with your long-term health.
Before you eat, pause for ten seconds and ask:
Relief want — Am I reaching for wine or sugar just to take the edge off?
Desperate want — Am I here because I skipped lunch and now my body is panicking?
Convenience want — Am I grabbing fast food because it’s easy, not because it’s what I need?
Aligned want — Am I choosing the harder meal that actually steadies me?
Most people never stop to ask.
But that ten-second pause is the difference between food running your life and you taking authorship.
Why Most Diets Collapse
This is also why cookie-cutter diets implode the moment life gets messy. They’re written for macros and aesthetics, not for stressed physiology.
But stress changes the rules:
Wired (anxious, restless) → needs steady protein + slow carbs to calm adrenaline.
Tired (burned out, flat) → needs nutrient density + gut support to restore energy.
Overstimulated (dopamine rollercoaster) → needs balanced glucose to stop the crash-cycle.
These aren’t medical diagnoses — they’re patterns in how stress shows up in the body.
Ignore them, and no plan sticks. (Read more about the 3 Neurotypes here)
Align with them, and food stops fueling stress and starts lowering it.
A Practical Checklist
Stress management isn’t just about what you practice with your mind.
It’s also about what you give your body to work with.
Food won’t erase stress.
But it decides whether your system calms down steadily — or keeps swinging between relief and chaos.
Stabilizers:
Protein-rich breakfasts (20–30g+).
Carbs always paired with protein/fat.
Omega-3s, magnesium, and colorful produce.
Steady, balanced meals across the day.
Agitators:
High-sugar meals on an empty stomach.
Processed oils and nutrient gaps.
Skipping meals or crash dieting.
Excess caffeine and alcohol.
Consistency matters more than perfection. The point isn’t to never stress eat. It’s to build a base that keeps you from crashing so hard, so often.
The Gavel Drop
Your nervous system doesn’t care about your intentions.
It cares about what you feed it.
Every meal either helps your system stabilize — or sets you up for another swing.
That difference shows up in how steady you feel, how clear you think, and how much stress hijacks your reactions.
Food isn’t just fuel.
It’s the fork before the fix.
The foundation that makes therapy and mindset work.
Feed your biology, because the body comes first.
Choose fuel that steadies you.
Download the FREE Stress Reset Nutrition Guide.
References
McEwen, B. S., & Akil, H. (2020). Revisiting allostasis and allostatic load: Implications for stress and brain health. Neuroscience & Biobehavioral Reviews, 119, 442–449. https://doi.org/10.1016/j.neubiorev.2020.09.008
González-Bono, E., Rohleder, N., Hellhammer, D. H., Salvador, A., & Kirschbaum, C. (2002). Glucose but not protein or fat load amplifies the cortisol response to psychosocial stress. Hormones and Behavior, 41(3), 328–333. https://doi.org/10.1006/hbeh.2002.1766
Witbracht, M., Keim, N. L., Forester, S., Widaman, A., & Laugero, K. (2015). Female breakfast skippers display a disrupted cortisol rhythm and elevated blood pressure. Physiology & Behavior, 140, 215–221. https://doi.org/10.1016/j.physbeh.2014.12.044
Jacka, F. N., O’Neil, A., Opie, R., Itsiopoulos, C., Cotton, S., Mohebbi, M., ... & Berk, M. (2017). A randomized controlled trial of dietary improvement for adults with major depression (the “SMILES” trial). BMC Medicine, 15, 23. https://doi.org/10.1186/s12916-017-0791-y
Liao, Y., Xie, B., Zhang, H., He, Q., Guo, L., Subramaniapillai, M., ... & McIntyre, R. S. (2019). Efficacy of omega-3 PUFAs in depression: A meta-analysis. Translational Psychiatry, 9, 190. https://doi.org/10.1038/s41398-019-0515-5
Moabedi, Y., Ettefagh, M., & Farhangi, M. A. (2023). The effect of magnesium supplementation on depression, anxiety, and stress: A systematic review and dose–response meta-analysis. Nutrients, 15(2), 325. https://doi.org/10.3390/nu15020325
Bae, J. H., Kim, L. K., Min, S. H., Ahn, C. H., & Cho, Y. M. (2018). Impact of premeal whey protein on postprandial glycemia and satiety in type 2 diabetes: A randomized crossover trial. Diabetes Care, 41(6), 1212–1218. https://doi.org/10.2337/dc17-2687